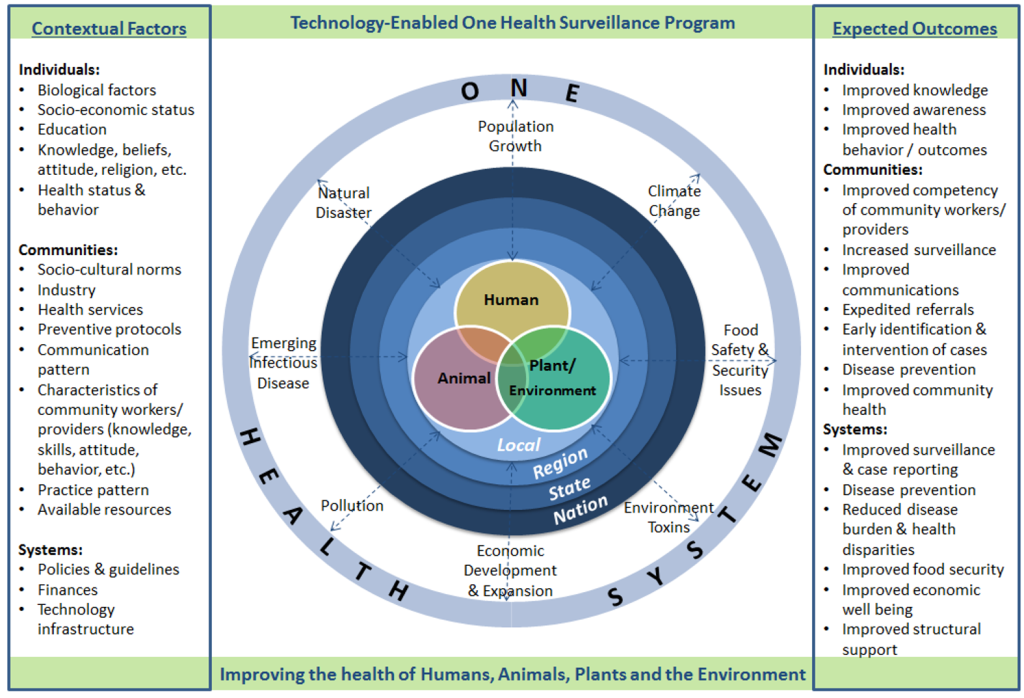
Environmental pressures, climate change, population growth, and food security issues have created health problems that require a multidisciplinary One Health (OH) approach to finding solutions. One Health is the term that refers to the collaboration of multiple disciplines working locally, nationally, and globally to attain optimal health for people, animals, plants, and the environment [1]. In this viewpoint we outline a community-based approach to monitor and improve early detection of OH problems to improve health.
Emerging and re-emerging zoonoses (Ebola and Nipah viruses, Middle East Respiratory Syndrome (MERS)), and diseases in plant species (Taro leaf blight, wheat head blight) have shown how vulnerable humans are to diseases that impact our health either directly or through their consequences on food safety and security [2-5].
Infectious diseases are not the only OH concern affecting human, animal, and plant health. Waste and toxins dumped in, or near, water sources contaminate streams, rivers, and lakes affect crops, animals, and people. Economic pressures to increase agricultural production contribute to global warming with resultant changes in weather that decrease freshwater supplies, and change microbial patterns [6]. Moving forward, a focus on promoting human health depends on expanding from a human centric perspective to a broader OH perspective with attention on the interdependence between humans, animals, plants, and the environment.
Community health workers
Around the world, in countries such as Rwanda, Ethiopia, Sri Lanka, and the USA community health workers (CHWs) have become the frontline health care providers who share a culture, language, and customs with the local community. Their jobs vary as they deliver or monitor treatments, engage in the detection of common illness such as malaria and HIV, and offer preventive care through immunization, and maternal and child health. While CHWs function in their communities to provide limited primary preventive and curative services they direct their attention exclusively at humans with little attention given to animal, plant, and environmental health interfaces.
Globally, there is an urgent need for CHWs. Despite decades of providing services at the frontlines, CHWs often still function in a grey area of health care delivery and are often under-trained and undersupported. CHWs need additional training and supervision and access to high-quality health information that can be achieved using technology such as mobile devices capable of providing just-in-time information and improved communication with higher level providers.
Limited access to veterinary health services has not only had a negative impact on livestock production with implications for food security, but has led to the inappropriate and indiscriminate use of antibiotics given to animals by lay people struggling to manage animal health [7]. In rural areas, there have also been attempts to provide agricultural advice, often through agricultural extension services to assist farmers in increasing yield production and reducing the use of harmful pesticides [6,8]. Inappropriate use of pesticides and other agro-products that are toxic to animals and humans often enter the soil or water supply through misuse [9]. This lack of health integration across human, animal, plant, and environmental health sectors in an ever-shrinking world with landscape degradation and decreased access to natural resources begs for a shift in health services.
A new paradigm for community health workers
What if the CHWs’ job is shifted from an entirely human focus to one with a OH focus that provides support across all four domains, human, animal, plant/crop, and the environment? What if rather than being trained to deliver advice and treatment based on their own knowledge and memory recall, CHWs could rely on technology to provide evidence-based recommendations around human, animal and environmental/crop syndromes, tailored to local or regional health concerns, while also collecting and recording data that could be forwarded to district or national disease monitoring centers for early outbreak detection?
Globally, the World Health Organization (WHO) estimates that more than 400 million people lack access to health providers and basic health care services [10]. This gap is far larger when considering access to veterinary health and agricultural services. To meet this challenge our international team has developed a human workforce innovation – a new model of CHWs termed a “One Health Worker” (OHW) with two objectives: 1) addressing basic human, animal, crop/plant, and environmental health issues at the community level, and 2) early identification of emerging or pandemic disease threats.
One Health System
In most rural areas in low and middle-income countries the detection of, and response to, important diseases is slow and fraught with problems related to: 1) accurate data collection over wide geographic areas, 2) poor inter- and intra- professional communication, and 3) the inability to rapidly aggregate data into a useable format to show potential disease outbreaks.
mHealth tools have been shown to guide health care workers through the collection of surveillance data and the dissemination of “just in time” prompts and recommendations on a variety of specific diseases (diabetes, depression, HIV). The expanded use of mobile technology is a worldwide phenomenon both in and outside of health care, but this technology has not been utilized in the community setting by lay health workers to provide/collect data on adverse health events affecting human, animals, crops, and local environmental issues [11]. Advantages of mHealth technology for providing “just-in-time” health guidance to OHWs include timelier care, a higher quality of evidence-based care, and more rapid resolution of problems. There are also enormous benefits in being able to ‘geo-tag’ data through the global positioning system (GPS) to allow for the collection, surveillance and monitoring of incoming data related to humans, animals, and crops at the family, household, and community level.
We have developed a training course, materials, and an interactive mobile application (APP) to expand and support the integration of a OH workforce in the community. Our mHealth APP uses a simple user interface with a pictorially driven menu protocol. Behind the scenes a web-based tool follows algorithms as it aggregates data input from all the OHWs and pushes that data out such that it can be combined with climate variables, land cover changes, and administrative data, to create a geo-linked dashboard of syndromes that may indicate potential outbreaks and overlap in space and time across the human, animal, plant, and environmental sectors. The dashboard displays problem areas for evaluation by municipal, regional, or national level agency experts across sectors, for possible early intervention and follow-up where warranted. For complex problems or serious outbreak concerns, messages, photos, and history of the problem can be sent by supervising nurses to the respective human, animal, or plant experts who can opt to advise the OHW via text message or visit the household or family where the problem(s) has been detected. The advantage of our innovative system is that it can: 1) aid in providing surveillance coverage to a large area using existing, locally based, human resources, 2) be easily scaled and adapted regionally, and 3) includes numerous human, animal, and plant/crop diseases that impact the community, region, and nation.
The Philippine government, like many others, is faced with important health challenges including the shortage of well-trained and equitably deployed health workers, particularly in geographically isolated rural regions where 56% of the population resides [12]. Demands for living space, clean water, food security, animal health, crop productivity, and clean, inexpensive energy pose enormous social and economic challenges that have significant impacts on human health and well-being [6]. Large regions of the country have limited access to primary care and even fewer have access to expertise for animal or plant health. Furthermore, rural populations often have no reliable form of transportation to access health care.
Implementation of a one health surveillance program
The goal of the Philippine government is to improve health through early detection, intervention, and evaluation of OH problems. One important step is the development of a OH workforce guided by the training and technological resources based on internationally accepted evidence-based recommendations.
Uniting a OH workforce with APP-based technology will allow for data to be aggregated daily and examined via a web-based dashboard to identify trends and patterns and that are also linked to environmental impacts (eg, climate, landscape). Table 1 lists three examples of OH problems in the Philippines that impact humans, animals, and agriculture/environment. The problems include the avian flu, Japanese encephalitis, and pesticide exposure, and suggests how a OH Workforce, had they been available, might have provided benefit to human health.
| Example | Description of adverse one-health event | Impact on Humans | Impact on animals | Impact on agriculture / environment | Role that One Health Workers might have played |
|---|---|---|---|---|---|
| Avian flu: | |||||
| Overview: On the animal front, OHWs will use their mobile APP to collect data that will be useful to understand the community’s relationship with animals, approaches used in animal husbandry, and management of animals used for food consumption. The mHealth technology provides algorithms to address common animal problems. | In the Philippines, during late 2017, an outbreak of H5N6 avian flu (eg, bird flu) affected vast numbers of poultry. The occurrence started six months earlier in the spring of 2017 with a small number of backyard farmers who were raising quail. Their small flock infections quickly turned into the first avian flu outbreak recorded in the Philippines. It is not known how the avian flu started in the Philippines, but suspicion has focused on either migratory birds or the smuggling of ducks. | Potential for pathogenic avian influenza transmission to humans | Transmission among poultry (domestic and wild) | Decreased domestic avian flocks across a wide region | Early detection of sick birds at the family farm level and monitoring of disease spread |
| Potential impact on human morbidity and mortality | Culling of fowl | Early detection of flu-like symptoms in other animal species (eg, swine, horses, etc.) | |||
| Decreased food security across broad social groups with a larger impact in poorer more rural areas | Transmission to other domestic species (swine, canine, equine) requiring quarantine measures | Early detection of flu-like illness in humans | |||
| Eventually 600 000 birds were culled costing the economy an estimated $44 million in direct costs and this value does not include unmeasurable costs of loss of substantial protein from the diet for countless families. The military was mobilized to assist with massive culling and quarantine efforts. Trade bans by foreign countries were imposed on Philippine poultry. | Economic impact on backyard producers, mid-size producers and large poultry commercial enterprises from large culls | Transmission to diverse wildlife species | |||
| Supply and demand initially leading to decreases poultry prices followed by large increases in prices that impact family purchases | |||||
| Ban of poultry products by trading partners (eg, Japan, Saudi Arabia, Singapore, and South Korea) | |||||
| Loss of family farm income from days lost from work | |||||
| Over-reaction/panic by the public | |||||
| Japanese encephalitis: | |||||
| Overview: On the human side of the OH triad, OHWs seek to narrow health care disparities as they engage in regular house to house surveillance for acute illness (including pregnancies, births and deaths) and provide health advice/education. OHWs provide just-in-time health advice using the evidence-based mHealth device that guides them through algorithms, and ultimately to timely referrals to the appropriate provider (community clinic, district clinic, or hospital) with electronic data transmitted to the health care delivery facility. | Japanese encephalitis (JE) is the most important cause of viral encephalitis in Asia. Caused by a mosquito-borne flavivirus, it belongs to the same genus as dengue, yellow fever, and West Nile viruses. The disease is passed to humans through the bite of the Culex tritaeniorhynchus mosquito, which is active during day and night. Like other mosquito-borne diseases, cases of Japanese encephalitis tend to increase during the rainy season. In the Philippines, JE is endemic with an extensive geographic distribution but with a predominance in rural areas. JE predominantly affects children under 15 years of age. Six to seven percent of cases result in death. There is a strong need for early population-based surveillance to augment hospital reporting of cases. Persons bitten by this mosquito may not develop symptoms until 5 to 15 days after being bitten. Symptoms include fever, chills, headache, fatigue, nausea, vomiting, and confusion. Severe cases include neck stiffness, seizures, paralysis, and comatose that may lead to death. | Clinical impact on morbidity and mortality | Virus transmitted by mosquitos between wild avian species (eg, water birds), humans, pigs, and horses. | Minimize standing water | Early detection of clinical symptoms in horses, pigs, etc. |
| Mortality rate of 30% | |||||
| Serious long-term morbidity of 20%-30% | |||||
| Economic costs from days lost of work for adults and/or child minders | Disease in horses, donkeys, and pigs | Early detection of clinical symptoms in humans | |||
| Disproportionately impacting rural poor | Abortion and stillbirths in swine | Educational programs and community outreach to minimize mosquito breeding grounds and personal protection (attire, bed nets, avoidance of mosquitoes) | |||
| Wide ability to infect other animals without resultant disease | |||||
| Environmental Pesticide Exposure: | |||||
| Overview: In the Philippines, many rural households have gardens or reside close to cultivated crop and 25% of the Filipinos are employed in plant agriculture [13]. In the Philippines cultivation of these crops often demands fertilizer and pesticide use to manage pests and optimize crop yields [14]. The OHW will identify patterns of specific pesticide or fertilizer use, and help in the early detection of plant/crop diseases and/or crop failures. With the guidance of their mobile app, and access to agricultural expertise at the academic or district level, community-based OHWs will provide monitoring and advice for plants and crops. | In the Philippines agriculture contributes a large part to the gross domestic product. In developing countries including the Philippines there is a heavy reliance on pesticides to promote agricultural production. Pesticides are commonly organophosphates, carbamates, pyrethroid, and organochlorines. Organophosphate pesticides are the most popular pesticides with a major risk coming from DDT (dichloro-diphenyltrichloroethane). The major Philippines agricultural products are rice, corn, coconuts, and bananas in addition to livestock and poultry. School children often start working in the vegetable gardens as early as 6–9 y old they shovel soil, prepare land, plant, water, and apply fertilizers and pesticides. Pesticide poisoning is a major global health problem. As result of intentional, accidental, and occupational exposures, in excess of 5 million deaths from pesticides occur globally. More than 60% of pesticide poisoning victims are between 10 and 35 y old but pesticide poisoning is also common among children and infants. In Benguet province, the vegetable capital of the Philippines, 2000 vegetable farmers presented with complaints allergic skin and eye reactions, abdominal pain, dizziness, chest pain, headache and nose bleeding in 2005. The more time a person spent working in the fields the more serious their symptoms. Farmers presented with symptoms that often went unreported to health authorities because they failed to recognize the link between the pesticide exposures and their symptoms. | Clinical impact on morbidity and mortality on children, young adults, and farmers | Contamination of animals through water and inhalation. | Contamination of plants, rivers, water sources including wells through leaked agrochemicals. | Government agencies would benefit from an intensified surveillance system of both household and commercial agricultural pesticides. |
| Consumption of contaminated food products | Potential impact of food chain impacting food safety. | Routine surveillance leads to early detection of farmers’ clinical symptoms | |||
| Economic impact on backyard producers | Early treatment and control to minimize exposures and subsequent harms | ||||
| Educational programs / community engagement to promote awareness of safe pesticide use and storage | |||||
A OH approach needs to start at the community level where there is a strong need for OH data collection and health information dissemination by individuals trusted by the community. Our innovative OH approach has the potential to bring a trained workforce equipped with mHealth technology to rural communities to improve the health of people, animals, plants, and the environment. The benefits of a OH workforce are vital for surveillance of emerging diseases and chronic health problems across all sectors with attention to the benefits on human health. The systematic collection of data, and daily compilation of that data using geo-tagged mapping provides a potential to improve disease surveillance and detection, decrease lag time in response, and enhance monitoring of outcomes. Given the interconnectedness of our global community in which humans, animals, plants, and the environment impact each other and do not respect geopolitical boundaries, we believe it is time for training a community-based OH workforce coupled with technology to maximize their effectiveness.