In the year 2000 several countries committed to decrease maternal mortality implementing various strategies, including improved access to contraception, to achieve the Millennium Development Goal number 5 aimed at improving maternal health [1]. Despite the increase of 61 million adolescent girls with their demand for contraception satisfied with modern methods since 1990 [2], around 23 million adolescent girls annually are at high risk of unintended pregnancies [3]. In 2016, almost half of the 21 million pregnancies estimated in low- and middle-income countries in individuals aged 15-19 years were unintended, ranging from ~ 50% in Africa and Asia up to around 75%in Latin America [3].
Teenage births result in health consequences; children are more likely to be born pre-term, have lower birth weight, and higher neonatal mortality, while mothers experience greater rates of post-partum depression and are less likely to initiate breastfeeding [4,5]. Additionally, adolescent mothers face higher risks of eclampsia, puerperal endometritis, and systemic infections than older women aged 20 to 24 years [6].
Adolescent pregnancy can also have negative economic and social effect on girls and their families, with unmarried pregnant girls likely facing stigma and rejection by parents and peers [7]. With regards to education, school-leaving is often the direct cause of pregnancy: an estimated 5% to 33% of girls who drop out of school in some countries do so because of early pregnancy or marriage [7], which perpetuates the cycle of poverty because of fewer skills and opportunities for employment.
Literature has provided evidence of the association between the uptake of modern contraceptives and socio-economic determinants: living in urban contexts is linked to higher usage when compared to rural residence [8]. Similarly, older, wealthier [9] and higher educated women are more likely to use modern methods of contraception when compared to their counterparts [10]. Adolescents who are not married can face several barriers to access and use contraceptives because sexual activity is only considered acceptable within marriage in many settings [11]. Married adolescents, on the other hand, are often under pressure to have a child soon after marriage and end up pregnant at early ages [11]. Furthermore, partner disapproval of modern contraceptive use, can affect the adoption of modern contraceptives [12].
While considerable research has been conducted to explore use and barriers to use of contraception, no analysis is available on the estimated impact of unmet need for contraception among adolescent girls in low- and middle-income countries. This study estimates the effect of the lack of use of modern methods of contraception (MMC) on unintended pregnancies by assessing the usage of MMC in comparison with traditional methods and with non-use of contraception.
Data sources
Demographic and Health Surveys (DHS) are large, nationally representative household surveys regularly conducted since the year 1984 in over 90 low- and middle-income countries worldwide [13].
DHS use standardized measurement tools and techniques to ensure comparability across diverse sites and time-periods, and consist of different questionnaires, including a household and a women’s modules [14]. The latter is administered to women of reproductive age (ie, 15–49 years) and includes a contraceptive history calendar for the five years prior to the survey [15].
Since 2010, 36 latest country DHS have incorporated questions regarding contraceptive failure for the current pregnancy, which enables to differentiate from contraception discontinuation followed by early conception.
The answers “later” and “no more” to the DHS question ‘Did you want to have a baby later on or did you not want any (more) children?” were used to construct the variable “wanting to have no more children’ for the currently pregnant girls. Similarly, the answer “no” to the DHS question “Are you currently doing something or using any method to delay or avoid getting pregnant?” and the answers “no more children” and “no children within the next two years” to the question “Would you like to have (a/another) child?” were used to construct the variable ‘not desiring pregnancy and not desiring contraception’ for the currently non-pregnant girls.
Out of the total 36 DHS, 24 surveys were excluded because of the very small sample (fewer than ten) of current unintended pregnancies among girls.
Variables
The use of contraception was categorized into the following three categories: 1) MMC, including combined oral contraceptives, progestin-only pills, implants, injectable contraceptives, IUDs, male and female condoms, sterilization and LAM [16], 2) traditional methods, including withdrawal and fertility-awareness methods [16], and 3) non-use.
We defined ‘sexually active’ those females engaging in sexual intercourse/s within 30 days of the interview and unintended pregnancy as a pregnancy desired later after occurrence or not desired at all. While status of contraceptive usage for currently non-pregnant women was used at the time of the survey, contraceptive usage for currently pregnant referred to its use immediately prior the information on pregnancy, thus representing contraceptive failure.
Every pregnant woman who discontinued contraception selected one out of six categories primary reason for doing so. ‘Side-effects’ included hormonal contraception-related adverse events; ‘Health concern’ included belief of interference with human physiology; ‘Opposition’ included marital opposition to contraception. ‘Access’ included lack of awareness on how to purchase contraceptives. ‘Inconvenient’ included use-related discomfort. ‘Other’ included less prevalent reasons, such as ‘low sexual frequency and ‘spousal separation.
Study population and sample size
The risk of unintended pregnancy was computed including currently unintended pregnancies (n = 7268) among 15-19 year-old females and sexually active, currently not pregnant, 15-19 year-old women who did not desire to be pregnant (n = 121 894) at the time of survey. Data were collected in the following 12 countries: Bangladesh 2014, Colombia 2015, Honduras 2011/12, India 2015/16, Liberia 2013, Mozambique 2011, Namibia 2013, Niger 2012, Peru 2012, Sierra Leone 2013, Uganda 2016, and Zambia 2013.
Statistical analysis
In consideration of the DHS survey design, we accounted for clustering of women’s households by primary sampling units and included country random effect in the analysis.
We tabulated the country specific overall and adolescent female population together with each 15-19 year-old female survey sample size. We also calculated the overall and each country proportion of unintended pregnancies out of all current pregnancies and the proportion of non-desiring children out of all currently non-pregnant girls.
Overall use of modern methods of contraception, traditional methods of contraception and non-use of contraception were calculated for both categories of girl under-study (current unintended pregnancy and currently non-pregnant non-desiring children).
For each country and the pooled analysis, the risk (odds ratio (OR) and adjusted OR (aOR) of unintended pregnancy was assessed in relation to the type of contraception. Logistic regression models included residence (urban or rural), marital status, and wealth (poorest, poor, middle, rich and richest) [17] as covariates. P-values less than 0.05 were considered to keep variables in the model.
Adolescent population and adolescent birth rates by country were retrieved from UNICEF State of The World’s Children 2017 Statistical Tables in order to estimate annual expected pregnancies [18]. The estimated number of annual expected pregnancies was calculated as the number of adolescents multiplied by the adolescent birth rate and then by 1.15 to adjust for miscarriages and terminations [19].
Expected unintended pregnancies and population attributable fraction (PAF) of unintended pregnancies attributable to not using MMC were calculated for each country: P(E)(OR–1)/[1+p(E)(OR–1)], where P(E) was the proportion of unintended pregnancies due to non-use of MMC, OR the odds ratio of pregnancy and the use of MMC.
The PAF would provide the proportional reduction in undesired pregnancies if traditional methods of contraception and non-use of contraception at all were replaced by MMC.
The statistical software STATA 13.1 SE was used to perform statistical computations [20].
This analysis did not require additional ethical approval. The analysis relied upon publicly available data set with no identifying data to guarantee participant anonymity. Ethics approval for the survey was obtained by the institutional review board of ORC Macro (Calverton, MD, USA) and country health authorities.
A total of 30 595 out of 121 894 (25.1%) non-pregnant sexually active women who did not want any future pregnancy were exposed to contraception methods. The analysis evaluating reasons for discontinuing MMC included all adolescent women who discontinued for all reasons but failure. The response rate for fertility preference and intention to use contraception in the non-pregnant women population was >98.0% for all DHS countries.
Of 7268 unintended pregnancies the highest and lowest frequencies were in Peru (113, 71.5%) and Niger (164, 17.8%). Of the 121 894 not pregnant girls who did not desire pregnancy, Mozambique (1367, 50.7%) and Peru 4132 (94.1%) were the less and most represented, respectively (Table 1).
| Country DHS | Total country population (total female adolescent population) | Sample size 15-19 y old | Current unintended pregnancy, n (%) | Currently non-pregnant, adolescent not desiring children, n (%) |
|---|---|---|---|---|
| Bangladesh 2014 | 162 952 000 (16 261 000) | 1 944 | 90 (26.3) | 1182 (71.1) |
| Colombia 2015 | 48 653 000 (4 078 000) | 6 604 | 210 (69.2) | 5827 (89.3) |
| Honduras 2011/12 | 9 113 000 (995 000) | 5 227 | 132 (38.9) | 4220 (85.9) |
| India 2015/16 | 1 324 171 000 (125 043 000) | 134 751 | 5927 (29.6) | 88 872 (88.1) |
| Liberia 2013 | 4 614 000 (521 000) | 1 915 | 109 (60.3) | 1171 (66.4) |
| Mozambique 2011 | 28 829 000 (3 326 000) | 3 065 | 104 (31.1) | 1367 (50.7) |
| Namibia 2013 | 2 480 000 (269 000) | 1 857 | 82 (65.2) | 1228 (69.9) |
| Niger 2012 | 20 673 000 (2 352 000) | 7 905 | 164 (17.8) | 5448 (71.3) |
| Peru 2012 | 31 774 000 (2 803 000) | 4 489 | 113 (71.5) | 4132 (94.1) |
| Sierra Leone 2013 | 7 396 000 (852 000) | 4 051 | 118 (46.8) | 4259 (80.3) |
| Uganda 2016 | 41 488 000 (4 810 000) | 2 122 | 77 (35.5) | 1403 (63.9) |
| Zambia 2013 | 16 591 000 (1 926 000) | 3 686 | 142 (55.5) | 2785 (73.7) |
DHS – Demographic and Health Survey, CI – confidence interval
A total of 712 (9.8%) were using MMC, 371 (5.1%) traditional methods of contraception, and 6185 (85.1%) were not using any methods of contraception immediately prior to the current unintended pregnancy. Among non-pregnant and not desiring children adolescent women, 28 401 (23.3%) were using MMC, 3413 (2.8%) traditional methods of contraception, and 90 080 (73.9%) were not using any methods of contraception.
In the pooled analysis, use of traditional methods or non-use of any methods was associated with an increased risk of having an unintended pregnancy (OR = 3.4, 95% confidence interval (CI) = 2.1-4.7; OR = 4.6, 95% CI = 2.6-6.6, respectively) (Figure 1 and Figure 2).
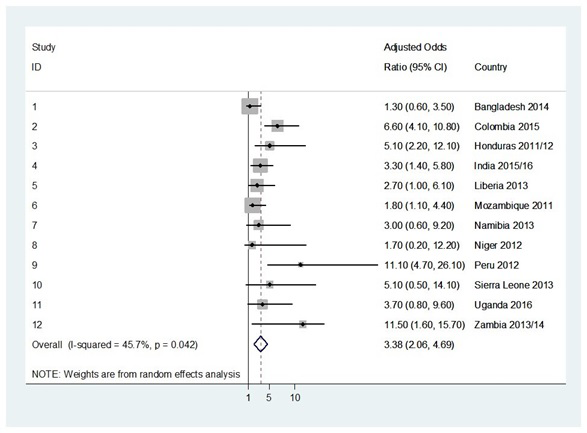
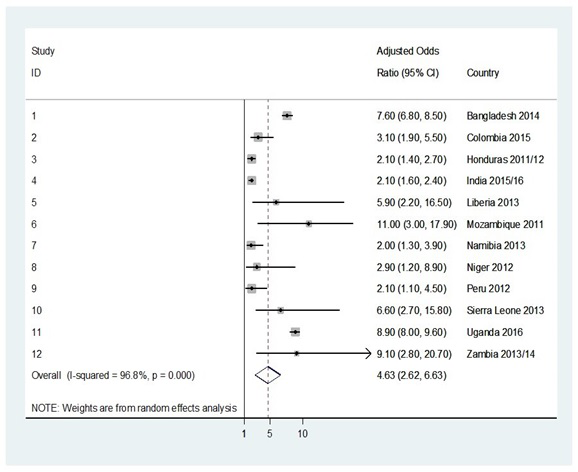
Country-specific OR of unintended pregnancy associated with using traditional methods ranged from 1.3 (95% CI = 0.6-3.5) for Bangladesh to 11.1 (95% CI = 4.7-26.1) for Peru, with statistically significant results for 7/12 (58.3%) countries. Country-specific OR of unintended pregnancy associated with the non-use of any contraception methods ranged from 2.0 (95% CI = 1.3-3.9) for Namibia to 11.0 (95% CI = 3.0-17.9) for Mozambique, with statistically significant findings for all 12 (100.0%) surveyed countries.
The PAF of not using MMC accounted for 86.8% (8 220 605) of the estimated unintended pregnancies (projected to be 9 464 654) in the pooled analysis. The PAF ranged from 65.8% (1 022 154) for Bangladesh to 95.1% (540 176) for Niger and the estimated number of unintended pregnancies because of the use of traditional methods or non-use of contraception ranged from 18 638 in Namibia to 4 303 872 in India (Table 2).
| Country, survey, years | Annual unintended pregnancies | Population attributable fraction (95% CI) | Number of annual unintended pregnancies due to non-use of MM |
|---|---|---|---|
| Pooled | 9 464 654 | 86.8 (85.4-88.3) | 8 220 605 (8 107 371-8 411 098) |
| Bangladesh 2014 | 1 554 642 | 65.8 (53.2-72.5) | 974 760 (814 632-1 145 771) |
| Colombia 2015 | 397 794 | 82.2 (80.0-84.4) | 326 987 (318 235-335 738) |
| Honduras 2011/12 | 113 281 | 89.8 (88.6-91.0) | 101 726 (100 367-103 085) |
| India 2015/16 | 4 608 179 | 93.4 (92.8-94.1) | 4 303 872 (4 201 112-4 373 341) |
| Liberia 2013 | 87 991 | 88.6 (87.3-89.9) | 77 960 (76 816-79 104) |
| Mozambique 2011 | 634 647 | 88.7 (87.2-89.6) | 562 932 (553 412-568 644) |
| Namibia 2013 | 24 174 | 77.1 (75.0-79.9) | 18 638 (18 130-19 315) |
| Niger 2012 | 568 008 | 95.1 (94.5-95.6) | 540 176 (536 767-543 016) |
| Peru 2012 | 219 195 | 92.7 (92.0-93.5) | 203 194 (201 659-204 947) |
| Sierra Leone 2013 | 128 354 | 82.4 (81.2-84.4) | 105 764 (104 223-108 331) |
| Uganda 2016 | 798 560 | 90.9 (89.5-92.8) | 712 263 (700 409-727 529) |
| Zambia 2013 | 329 832 | 89.5 (88.3-90.1) | 295 200 (291 242-297 179) |
CI – confidence interval, MM – modern methods
The study carried out in twelve low- and middle-income countries showed that ~ 9/10 unintended pregnancies would have been averted if MMC were utilized. The use of traditional methods and not using any methods of contraception significantly increased the odds of an unintended pregnancy, respectively.
Around 85% of adolescent women with a current unintended pregnancy and 75% of non-pregnant, not desiring children adolescent women were not using any contraception, which is the classical “unmet need” [21]. On the other hand, 5% and 3% of the two populations under study were making use of traditional methods, which entail a very high risk of unintended pregnancy as well as high STI/HIV exposure [22].
The surveyed countries record ~ 10 million unintended adolescent pregnancies annually, representing around 40% of the unintended pregnancies among adolescent women worldwide. In all countries adolescent girls had significant risk of unintended pregnancy associated with the non-use of contraception, whereas more than 50% had significant risk of unintended pregnancy associated with the traditional methods of contraception.
The high proportion (>¼) of women in Bangladesh and Namibia who became pregnant despite using MMC needs to be carefully evaluated. As emphasized by a 2014 policy brief, in Bangladesh there has been an important decline of the use of long-acting modern methods of contraception in the last decades; the increased adoption of short-acting modern methods of contraception and their incorrect use together with high rates of contraception discontinuation is slowing down the progress made in the past 20 years [23].
Furthermore, One out of four adolescent women with an unintended pregnancy discontinued MMC because of adverse events, confirming their role for discontinuation of drugs, injectables, and IUDs in low-income settings [24]. Discontinuation is a specifically important issue for adolescent due to the fact that they tend to have a more unpredictable and irregular sexual activity, more limited access than older individuals to family planning, and usually less knowledge about effective use of contraceptive methods [25]. More attention should be paid to social and health care factors, such as lack of access/availability and partner disapproval.
DHS are often the only nationally-representative source of reproductive health information in low- and middle-income countries and are generally considered of high accuracy [26]. However, DHS findings were compared across ten countries in different periods after 2005. However, standardized procedures and questionnaires were implemented minimizing the methodological variability [26].
More than 95% of the eligible women took part in all surveys under study, with Honduras having the lowest participation rates (95%) and Niger the highest (98%).
Post-event rationalization bias [27] on the intention status of pregnancies should have been minimized since with the analysis was focused on current pregnancies. Scientists have also argued on the validity of the meaning of “unintendedness”, following the contradiction on happiness pregnancy is diagnosed [28,29].
Further, the high heterogeneity within the category of unintended pregnancy should be carefully considered, with unwanted and mistimed pregnancies representing different life-choice considerations [30].
Moreover, recall bias on the contraception use prior to the current pregnancy could potentially affect the results [31]: women who experienced an unintended pregnancy might be more likely to recall and report their sexual behaviours compared with those who did not have any unintended pregnancy. Regular and frequent contraceptive use such as daily pill use, regular injections, or consistent use of an IUD could be expected to be more accurately recalled than coitally dependent methods such as condom use and withdrawal, which are practiced more sporadically and infrequently [32]. Underreporting of certain methods such as condoms has been in fact documented in different studies, especially in West Africa [33].
As showed by several reviews [34,35], adolescent face barriers in obtaining and using modern contraception in low- and middle-income settings (eg, drug shortages) [36,37]; furthermore, when they are available, health care workers and/or local policies cannot provide family planning services to adolescents or those under a certain age [36]. Stigma on contraception can prevent their use by adolescents not in stable relationship [38].
Fear and concerns related to misconception on early and long-term adverse events can lead young women to consider more acceptable withdrawal and other traditional methods [39].
Moreover, poor understanding of how contraceptives methods works, and consistent use of contraception has been shown to be problematic among adolescents [40]. Unintended pregnancies often occur during periods when women engage in contraceptive switching, often to less effective methods, or when abandon contraception [41,42]. The rate of switching to no method is key: 85% can become pregnant in the first year after stopping [43]. A DHS report showed that adolescent women are at high risk of discontinuation when compared to older women [44]. In this regard, consistent male condom’s use, which is the most commonly used method by adolescents due to accessibility and price [36], tends to decrease over time within stable partnerships [45].
A recent Cochrane review [46] showed that promoting the use of contraceptive measures did not reduce the risk of unintended pregnancies; however, multiple interventions (ie, educational, skill building and contraception promotion) can reduce the rate of unintended pregnancies in adolescents [47,48].
A recent study [49] underscored that 90% of adolescent women used short-acting methods (eg, condoms, pills, injectables) and that an increase in the use of long-acting reversible methods (eg, IUDs and implants) would decrease the cost.
In conclusion, our study estimated that 8 million unintended pregnancies in 12 low- and middle-income countries could have been prevented annually if all adolescent women who did not desire pregnancy had used modern methods of contraception. It is fundamental to understand how under use of MMC translates into a disease and mortality burden. Systematic efforts are needed to address issues like access to contraception, fear of adverse events, opposition to use and underestimation of the risk of pregnancy.
Combined approach with multi-sectoral approach including health facility (antenatal, immediate post-natal and post-abortive care visits), school (sexual education), national policies and laws, as well as the use of media describing accurate and context-tailored information, are recommended to advance towards the Sustainable Development Goal 3 [50]. This is also in line with the Universal Health Coverage Agenda, which specifically calls for the inclusion of core sexual and reproductive health in health services by providing a level of financial protection sufficient to insulate adolescent against economic hardship [51].














