Noncommunicable diseases (NCDs) have accounted for 68% of the world’s 56 million deaths in 2012 [1], with half of the people with NCDs having two or more conditions (multimorbidity) [2,3]. Multimorbidity is a comparatively new concept and a challenging area in medical practice globally. Although it is simply defined as “the coexistence of multiple chronic conditions in a given individual” [4,5], based on the research to date [2,3], there is no consensus on which conditions should be considered; or on the method used for measuring multimorbidity. This makes comparisons between– or among studies difficult.
With increasing population and life expectancy, the disease burden of multimorbidity to both individuals and society are increasing. Multimorbidity is already, and will be in the future, a great challenge for both developed– and developing country settings [3,5]. A staggering toll of about 80% of NCDs deaths occurred in low income settings [6], and the most socioeconomically deprived areas have substantially more multimorbidity, that happens earlier (10–15 years) than do their most affluent peers [2], however, evidence from low income settings is limited [3,7-9]. The identification and implementation of innovative approaches are essential for tackling this growing epidemic, especially for and in LMICs.
Better understanding of the whole picture of global research trends, activities and identification of the knowledge gaps on multimorbidity is necessary to move the research agenda forward, and especially for LMICs. This has coincided with the World Health Organization (WHO) global health and research priority on healthy aging [3,10]. While some studies have pointed to the mismatch between the importance of multimorbidity and research outputs in this area [11–13], only a few studies have comprehensively evaluated the research trends, knowledge gaps, and inequality among countries. We aimed to use a comprehensive bibliometric analysis to document these gaps at a global level.
Data sources and search strategy
A comprehensive search was conducted to identify research publications on multimorbidity including its various spellings (multiple chronic diseases, multiple chronic conditions, polymorbidity, polypathology, pluripathology, and multipathology) in the Web of ScienceTM, Core Collection database, one of the world largest databases of peer–reviewed literature provided by the Thomson Scientific Institute. The time frame for the search was from 1900 to June, 2016. Detailed search strategies can be found in Appendix S1 in Online Supplementary Document. The same search strategies were performed on four other leading causes of death: diabetes, depression, hypertension, and COPD. We included all publication types (such as, article, meeting abstracts, review, editorial, letter, etc.).
We also collected the life expectancy at birth (years) and gross national income (GNI) per capita from the website of the World Bank to examine the relationship between these variables and research outputs. The income groups included low–income (US$ 1025 or less), lower middle–income (US$ 1026 to US$ 4035), upper middle–income (US$ 4036 to US$ 12 475), and high–income (US$ 12 476 or more) economies based on per capita gross national income.
Data analysis and visualization
All publications were included with the following variables extracted: publication date, subject category, document type, author, organization of origin, funding agency, language, country of origin, title, abstract, and keyword. In addition, the full texts were obtained for the co–citation analysis. The retrieved results were exported to both Microsoft Office Excel (Microsoft, Seattle, WA, USA) and plain text for further analysis.
Data were linked with the life expectancy at birth (years) and GNI in Microsoft Office Excel. The Pearson correlation coefficient (r) between life expectancy at birth (year) and annual publications (on the logarithmic scale) was calculated.
CiteSpace II [14] was used to conduct co–citation and hierarchal clustering analysis to map the trends and research networks.
Characteristics of research landscapes on multimorbidity worldwide
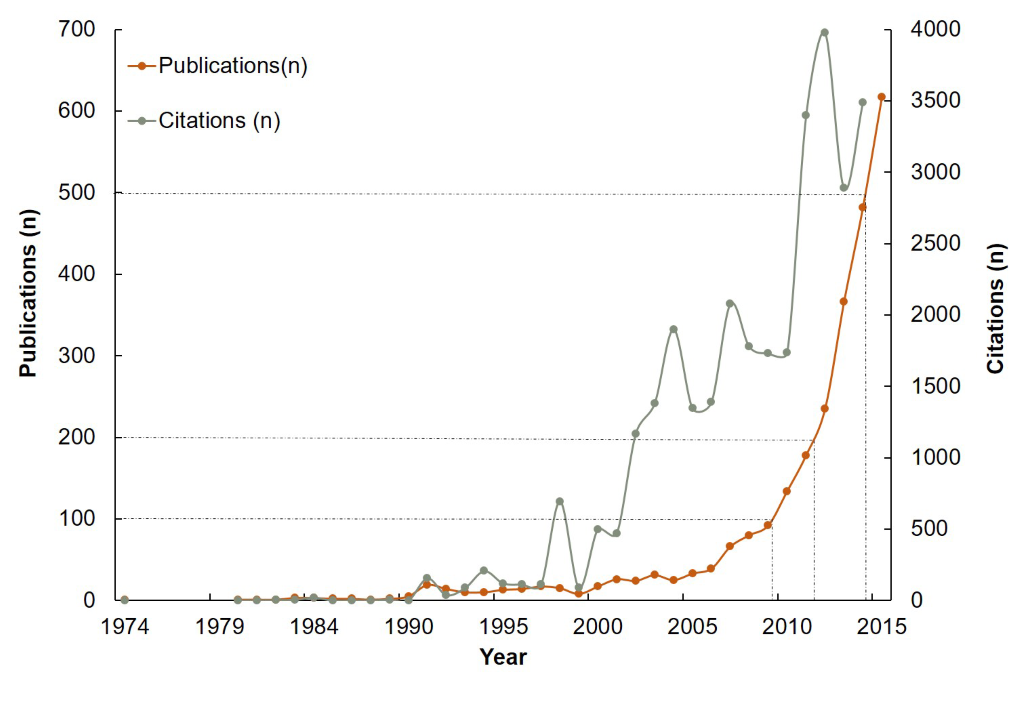
A total of 2864 articles on multimorbidity were retrieved from the database, with the first indexed in 1974 from Germany. As shown in Figure 1 , the publications appeared sporadically before 1990, and increased slowly up to the early 2000s, with a transition to exponential growth after 2005. Of the 2864 articles, 80% were published after 2010, while only 9% appeared between 1974 and 2004. Regarding the development of annual total citations, Figure 1 shows a similar trajectory to the publication data with a total of 31 669 citations. However, the exponential growth started around 2000.
The primary type of publication was research article (74%) (see Appendix S2 in Online Supplementary Document). There were 12 publication languages, 87% were reported in English, followed by German (10%), Spanish (1.3%) and French (1.0%) (see Appendix S3 in Online Supplementary Document). The publications covered 897 journals, and we identified the top 20 journals had published around or more than 20 articles between 1974 and 2016. Journals with the most articles on multimorbidity include the Journal of the American Geriatrics Society (n = 74), PLOS One (n = 74) and BMC Family Practice (n = 67). Further details on the top 20 journals can be found in Appendix S4 in Online Supplementary Document. Of the 20 most prolific authors, 15 were from Europe, four were from North America, and one was from Australia, with none from LMICs (see Appendix S5 in Online Supplementary Document).
Overall, the three leading research institutions (Johns Hopkins University, Harvard University, and University of California System) were from the US, followed by Germany and UK institutions (see Appendix S6 in Online Supplementary Document). Visualization of the institutions performance and collaborative networks can be seen in Appendix S7 in Online Supplementary Document. Nine of the top 15 funding agencies from US sponsored the most publications (see Appendix S8 in Online Supplementary Document).
A total of 117 different subject categories were involved in this research area, with the leading three subject categories: Medicine General Internal (691 papers), Health Care Sciences Services (422 papers), and Geriatrics Gerontology (381 papers). The top 20 subject categories are listed in Appendix S9 in Online Supplementary Document. The different subject categories connected broadly, imply that multimorbidity research is an interdisciplinary area (see Appendix S10 in Online Supplementary Document).
Knowledge Gap 1. Mismatch between the high prevalence of multimorbidity and its publication outputs
Compared with other high prevalence single chronic condition (diabetes, hypertension, depression, and COPD), there is a mismatch between the high prevalence of multimorbidity and its research outputs. Although the median prevalence of multimorbidity is 63%, the number of articles on the other four single conditions is 13 to 150 times that of multimorbidity ( Table 1 ).
| Conditions | Prevalence (year) | Publications | Ratio of articles on multimorbidity vs on other four conditions |
|---|---|---|---|
| Multimorbidity | 13%–83% (1989–2012) [15]* | 2864 | 1:1 |
| Diabetes | 9% (2014) [1] | 431 009 | 1:150 |
| Depression | 5.9–14.6 (2000s) [16] | 360 666 | 1:126 |
| Hypertension | 22% (2014) [1] | 346 894 | 1:121 |
| COPD | 11.7% (2010) [17] | 36 866 | 1:13 |
*A systematic review included articles from 1989 to 2012, with median prevalence 63%.
Further analysis demonstrated both physical and mental disorders are contained in the research framework of multimorbidity. Table 2 shows the top 10 featured conditions and leading risk factors mentioned in the keywords list. Similar findings were also found in other research types, such as systematic review [18], and longitudinal cohort study [19]. The leading disease and risk factor was cardiovascular and heart disease, and physical activity, respectively.
| Rank | Conditions or risk factors | Appearance (n) |
|---|---|---|
| Diseases: | ||
| 1 | Cardiovascular and heart disease | 340 |
| 2 | Depression | 195 |
| 3 | Diabetes mellitus | 94 |
| 4 | Dementia | 85 |
| 5 | COPD | 78 |
| 6 | Cancer | 70 |
| 7 | Hypertension | 56 |
| 8 | Alzheimer disease | 41 |
| 9 | Chronic kidney disease | 34 |
| 10 | Cognitive impairment | 33 |
| Risk factors: | ||
| 1 | Physical activity | 51 |
| 2 | Obesity | 45 |
| 3 | Body mass index | 30 |
Knowledge Gap 2. Imbalance in publications among countries and the roles of economics and life expectancy
Table 3 outlines indicators to demonstrate the imbalance in research outputs on multimorbidity and NCD disease burden and life expectancy. Compared with 73% NCD related deaths that occurred in LMICs, only 5% of publications on multimorbidity originated from LMICs. Onset of the median year of first publication occurred 15 years later in the LMICs compared with HICs (2010 vs 1995.), and at that time point, the life expectancy at birth (years) was 66.1, with the gap between LMICs and HICs 7.9 (68.4 vs 76.3).
| Indicators | Income group | |
|---|---|---|
| LMICs | HICs | |
| Multimorbidity publications (%) | 176 (5) | 3510 (95) |
| NCD deaths (%)* | 27 733 (73) | 10 159 (27) |
| Median year of the first publication | 2010 | 1995 |
| Life expectancy at birth (years) at the median year of the first publication | 68.4 | 76.3 |
LMIC – low– and middle–income countries, HIC – high–income countries
*Data sources: World Health Organization [20].
We analyzed the year of first publication and total number of publications by country. Figure 2 shows the distributions and trends of publications between 1974 and 2016 plotted according to the level of GNI per capita in 2015 for the 76 countries with at least one publication indexed in the Web of ScienceTM. The GNI data sources for Figure 2 are from the World Bank [21]. The chart illustrates the substantial knowledge gaps with a direct gradient apparent by income country status, especially compared with the disease burden ( Table 3 ).
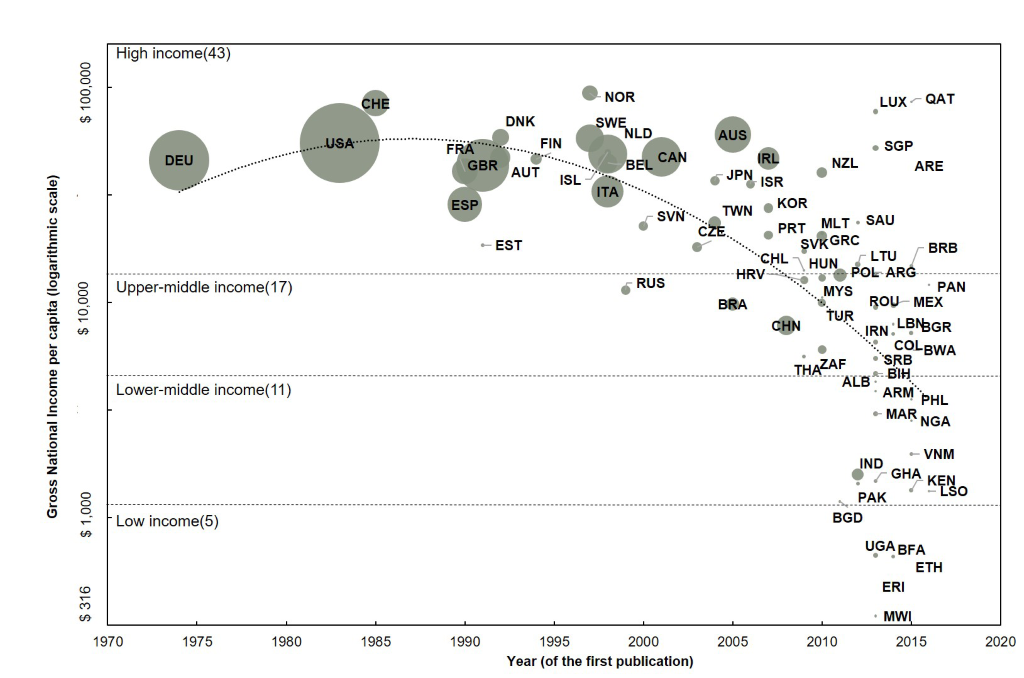
Among the income groups, there is a great deal of heterogeneity in the year of first publication and total number of publications. The number of countries in high income, upper–middle income, lower–middle income, and low–income countries is 43, 17, 11, and 5 respectively. Although Germany published earlier (1974), US holds the most publications (n = 895), followed by Germany (n = 511) and UK (n = 389). All the top 15 countries were HICs; the first LMIC being China with 52 publications, ranked 16th. The median year of the first publication in high income, upper–middle income, lower–middle income, and low income countries was 1995, 2010, 2013, and 2014 respectively. The first LMIC publication was in 2005 by Brazil, which is ranked 25th.
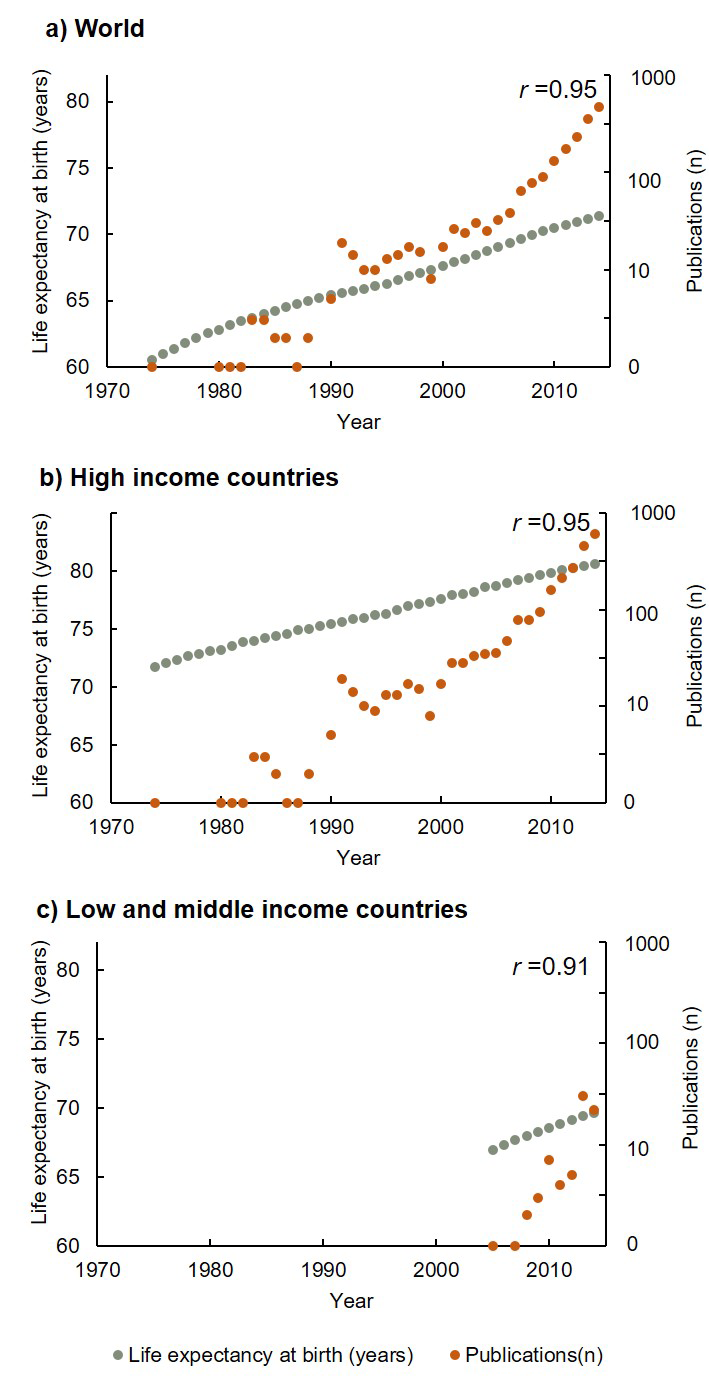
Figure 3 shows the relationship between life expectancy at birth (years) and annual publications (on the logarithmic scale) from 1974 through 2014. Longer life expectancy was associated with higher publication outputs in both HICs and LMICs (r = 0.95 and 0.91, respectively). The life expectancy at the median year (1994) of first publication was 66.1, with a gap between LMICs and HICs of 7.9 (68.4 vs 76.3). The data sources for Figure 3 are from the World Bank [22].
Applications: research topics evolution over time and potential collaborations between HICs and LMICs
Terms from keywords were used to explore the emerging research trends and evolution topics [14]. 152 distinct topics from keywords of publications were obtained between 1990 and 2016 to illustrate the rapidly advancing research area. Figure 4 shows the research topics evolution over the years, with topics beginning with depicting epidemiology characteristics (such as “prevalence”, “age”, “disease”, “disorders”, “chronic disease” and “mortality”), then moving to exploring risk factors, the impact of multimorbidty on individuals and the health system (such as “determinants”, “quality of life”, “family practice”, “self management”, “guideline”, “polypharmacy”, and “adherence”), and more recently examining interventions and how to improve the management (such as “intervention”, “education”, “comprehensive geriatric”, “collaborative and integrated care”).
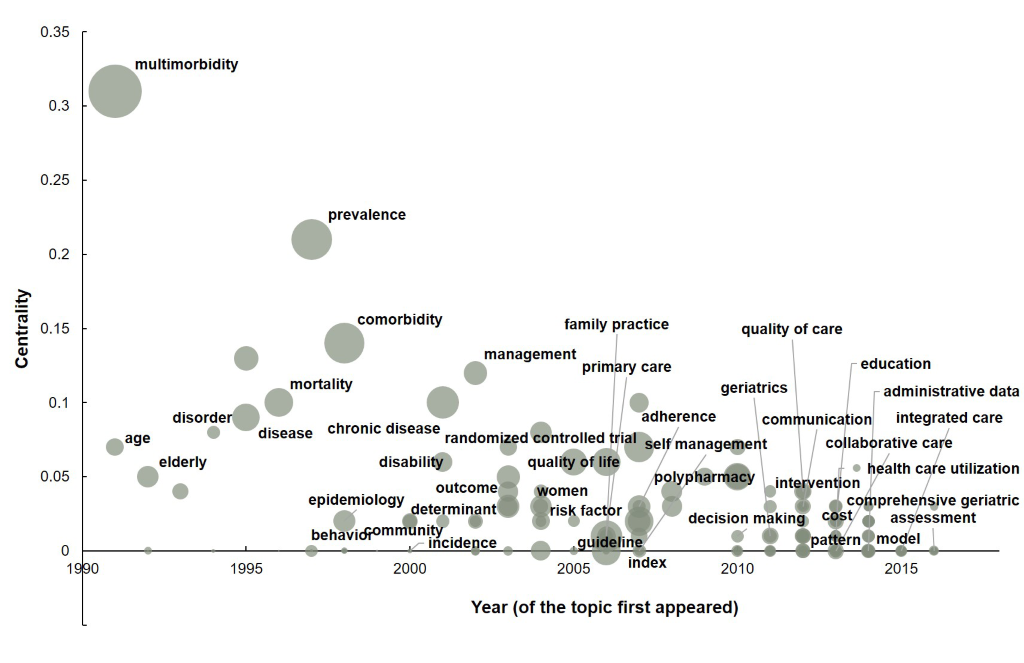
Figure 5 shows the featured research topics (based upon the top cited publications from each income group in each year) evolution in each income group between 2000 and 2016, in an attempt to illustrate the knowledge gaps and potential collaboration among countries (the full results of the featured publications and the top 15 cited publications can be found in Appendices S13 and S14 in Online Supplementary Document). Featured research topics in Figure 5 were based on the top cited publications from each income group in each year: high–income countries [2,13,23–36], upper–middle income countries [8,37–45], lower-middle income countries [7,9,46–50], and low–income countries [51–53].
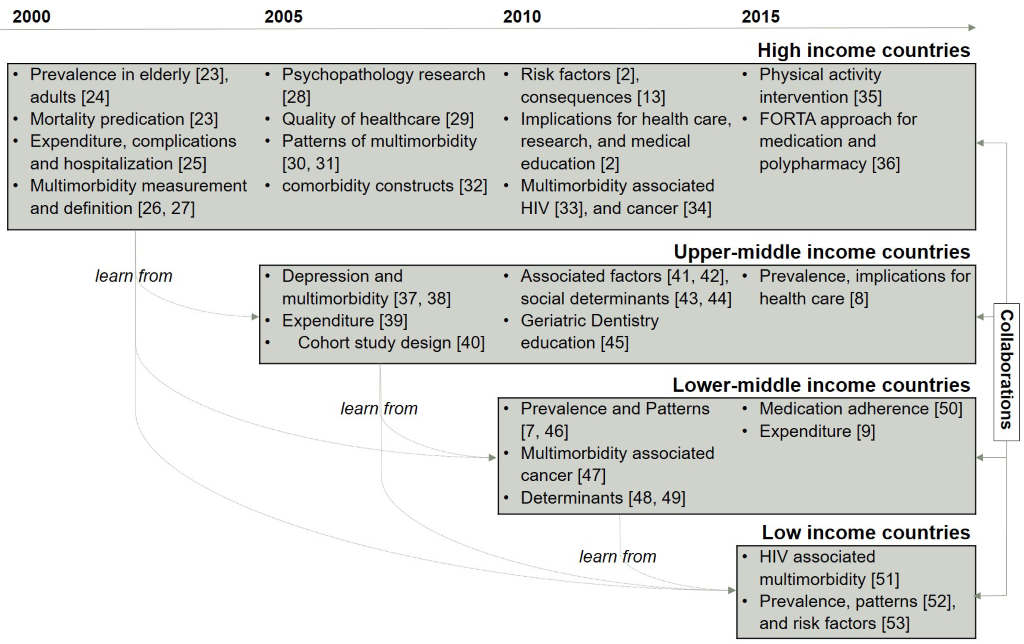
Most of the research topics evolution was similar among high and low income countries over time, especially in the initial stage when investigation began in this research area. It can be seen from the chart that HICs have contributed more knowledge than LMICs. If we take an epidemiology study as an example, HICs have published studies on “how to define and measure multimorbidity”. This research can potentially be used by other income group countries and tailored to fit their own contexts and populations. Other examples such as “multimorbidity associated HIV and cancer”, “physical activity intervention”, and “approaches for medication and polypharmacy” that had been investigated by HICs have only just emerged as a research topic in other countries.
As the figure shows, although collaborations have existed, such as in the FINE study (Finland, Italy, Netherlands) [23], and WHO’s Study on global Aging and adult health (SAGE) (China, Ghana, India, Mexico, Russia and South Africa) [9], these collaborations occurred within the same income groups. There were no collaborations between LMICs and HICs, however, potential collaborations between HICs and LMICs are possible.
According to the best of our knowledge, this is the first study to evaluate the knowledge gaps and the potential for collaborations on multimorbidity between LMICs and HICs. Although it is well recognized that multimorbidity is a neglected research topic, such as in clinical guidelines and in randomized controlled trails (RCTs) [54–59], two of our findings and one implication are largely new.
First, compared with single conditions (diabetes, hypertension, depression, and COPD), there is a mismatch between the high prevalence of multimorbidity and its research outputs at the global level. This finding was also identified by Fortin and co–workers in the Canadian population among people aged 55 to 74 years [11]. Research conducted by the Emerging Risk Factors Collaboration [60] examined 689 300 participants from 91 cohorts and concluded that increasing numbers of chronic conditions within individuals are multiplicatively associated with increased mortality risk. Facing this huge disease burden, there is only a limited evidence base on which to inform policy and practice for these urgent health care needed individuals [61].
Second, research knowledge on multimorbidity from LMICs is comparatively limited compared with HICs (5% vs 95%), whereas nearly 80% of NCD related deaths occurred in LMICs. However, during the past 5 years, the number of publications originating from LMICs has grown substantially. Most publications were from upper–middle income countries, especially Brazil and China. On further analysis, we found that economic status and life expectancy played important roles in this gap, with higher economic status and longer life expectancy positively associated with higher annual publication outputs and the median year of first publication. One large study from Scotland found that the onset of multimorbidity occurred 10–15 years earlier in people living in the most deprived areas compared with the most affluent [2]. This finding coincides with two interesting statistics from our study: (1) onset of the median year of first publication occurred 15 years later in the LMICs compared with HICs, and (2) the life expectancy at the median year of first publication in LMICs was 7.9 years lower than in HICs. The potential implications from these findings are that: people from lower socioeconomic settings are more vulnerable to multimorbidity; and multiple chronic conditions is especially debilitating in LMICs, where they are facing the double burden of communicable and non–communicable diseases where dealing with premature, infectious diseases and single conditions are already great challenges.
Higher income is associated with greater longevity, with differences in life expectancy across income groups increasing [62]. With life expectancy increasing over the world, especially in LMICs, it is estimated that 80% of older people will be living in LMICs by 2050. This leads to questions of whether we have accumulated enough knowledge at a pace that can meet this challenge, especially in LMICs, and what more can we do based on the latest knowledge.
Despite the paucity of studies indicating the lack of research capacity and funding, LMICs may benefit from the theoretical and practical experience of HICs in multimorbidity research and implementation. However, tremendous national and international effort is needed to address the knowledge gaps between countries and provide better evidence to inform medical and public health decisions needs. The barriers to implementation of knowledge and experience generated from HICs needs to be evaluated, with the purpose to develop better availability and affordability in multimorbidity control and prevention strategies and measures. Take integrated care as an example; although it can create efficiency gains and improve health outcomes [63], it may only apply to HICs with good health systems. For LMICs, challenges from capacity building, better quality services, and a stronger evidence base will be required for implementing integration of care [3,64], but this is feasible as demonstrated by some operational models and approaches, such as the WHO 25 × 25 strategy (a target of a 25% relative reduction in NCD mortality by 2025) and the Integrated Management of Adult and Adolescent Illness (IMAI) [65,66].
Our findings demonstrate significant gaps in multimorbidity research between HICs and LMICs with limited knowledge of etiology, epidemiology, patterns, progression, risk factors and efficacy and cost–effectiveness of different interventions [64,67]. Knowledge on polypharmacy is lacking, as most of the evidence generated from RCTs is of limited value to guide decisions about medication use by patients with multiple chronic diseases as the possible drug–to–drug, drug–to–disease, and disease–to–disease interactions remain unexamined [5].
Limitations
Several limitations are associated with our comprehensive bibliometric study. A linguistic bias may exist with the restriction to publications in English language journals. Second, in order to perform a high quality bibliometric analysis, we only searched the Web of Science database, which doesn’t include non–SCI journals, such as the Journal of Comorbidity, where there may be many multimorbidity relevant publications. In addition, we have not provided a detailed analysis of the research topics, such as the prevalence and disease burden of multimorbidity in each country or income group. In order to move the research agenda forward, we suggest topic specific systematic reviews which cover more databases, a secondary analysis of data at the global level, and primary longitudinal cohort studies are needed.
This study confirms substantial knowledge gaps in multimorbidity research and between HICs and LMICs countries, research agenda and inputs needed to move research forward worldwide, especially for and in LMICs. There is a possibility that LMICs can learn from and collaborate with HICs in this area.